IVF & Fertility Treatments
Following a comprehensive workup, our team of experts will identify the most suitable treatment plan tailored to your needs.
This personalized approach not only optimises your time and resources but also enhances your chances of achieving a successful outcome.
Assisted Reproductive Technology (ART) services available at Coastal IVF:
Ovulation Induction and Intra-Uterine Insemination (OI/ IUI)
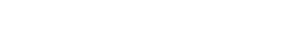
Ovulation Induction (OI) combined with Intra-Uterine Insemination (IUI) is a treatment that helps increase your chances of getting pregnant. OI uses oral medication or injections to stimulate the ovaries and promote ovulation. During this process, we closely monitor the development of the follicles with ultrasounds and blood tests. When the timing is right, a prepared sperm sample is placed directly into the uterus through IUI. This treatment is especially helpful for individuals with ovulation problems or mild male infertility.
In Vitro Fertilisation (IVF)
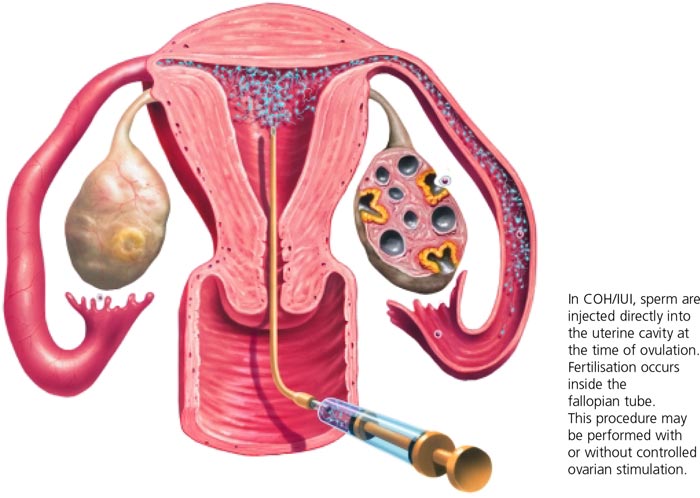
In Vitro Fertilization (IVF) is a fertility treatment that starts by using medications to stimulate the ovaries to grow multiple mature follicles (usually 10-20). Just before ovulation, these follicles are retrieved under anaesthesia to collect the eggs, or oocytes. In the laboratory, the oocytes are combined with sperm for fertilisation. After 3-5 days, the resulting early-stage embryos are assessed and then transferred to the woman’s uterus, with the hope of successful implantation and pregnancy.
IVF is a flexible option for various fertility challenges, such as blocked fallopian tubes, male infertility, and unexplained infertility. It can also involve the use of donor eggs or sperm and allows for genetic testing when needed.
Intra-Cytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection (ICSI) is a specialised type of In Vitro Fertilisation (IVF) that helps couples facing male infertility or fertilisation challenges. In this procedure, a single healthy sperm is directly injected into an egg (oocyte) to promote fertilisation. ICSI is especially useful in cases of low sperm count, poor sperm movement, or abnormal sperm shape. By overcoming many natural barriers to fertilisation, ICSI increases the chances of developing healthy embryos, making it an effective option for couples trying to conceive.
Pre Implantation Genetic Testing (PGT)
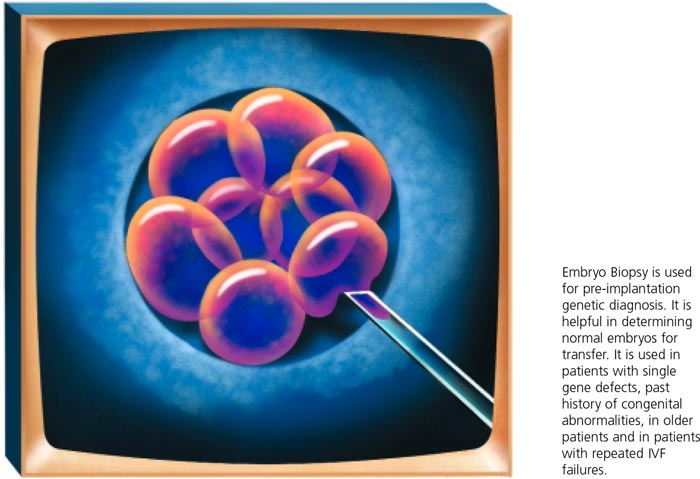
Preimplantation Genetic Testing (PGT) is an important procedure used with In Vitro Fertilisation (IVF) to detect genetic issues in embryos before they are placed in the uterus. During PGT, a few cells are gently taken from each embryo and tested for specific genetic conditions or chromosomal abnormalities. This testing is especially helpful for couples with a family history of genetic disorders, those who have had multiple pregnancy losses, or individuals of advanced maternal age. By choosing only the embryos without genetic problems, PGT increases the chances of a successful and healthy pregnancy (per transfer) while reducing the risk of inherited genetic diseases in the child.
Sperm, Oocyte and Embryo Freezing (cryopreservation)
Fertility preservation is a crucial option for individuals who want to protect their reproductive potential for the future. This process involves collecting and freezing sperm, oocytes (eggs), or embryos, so they can be stored until the individual is ready to conceive.
For men, sperm can be collected and frozen before medical treatments like chemotherapy, or for those who wish to delay fatherhood. Women can choose to freeze their oocytes, allowing them to preserve eggs for later use, which is particularly useful for those delaying childbearing for personal or medical reasons.
Additionally, couples undergoing IVF can opt to freeze viable embryos for future use. Fertility preservation offers peace of mind and flexibility, helping individuals and couples keep their family planning options open until the right time.
We understand that this information can feel overwhelming, but we’re here to support you in navigating your options and making the process as straightforward as possible.
If you would like more detailed information on various treatment options please see below
Treatments in Detail:
Ovulation Induction and Intra-Uterine Insemination
Ovulation induction (OI) is commonly utilised for women experiencing ovulation disorders, one of the leading causes of subfertility or infertility. Ovulation issues are particularly prevalent in women with conditions such as polycystic ovary syndrome (PCOS), endometriosis, and those of advanced age.
OI involves the use of oral medications to enhance the brain’s natural production of follicle-stimulating hormone (FSH), which is essential for recruiting and growing ovarian follicles. Regular ultrasounds are conducted to monitor follicular development. Once a dominant follicle reaches an adequate size, ovulation may either occur naturally or be triggered with an injection.
Approximately a day after ovulation, Intra-Uterine Insemination (IUI) is performed. This procedure involves preparing the sperm to concentrate healthy spermatozoa, which are then placed directly into the uterus using a soft catheter.
Pros and Cons of OI/ IUI:
Pros:
- Less invasive and requires fewer medications than IVF
- Significantly lower cost compared to IVF
- Minimal laboratory involvement, closely mimicking natural processes
Cons:
- Lower success rates (per cycle) compared to IVF
- Provides less diagnostic information than IVF, as it does not allow for assessment of fertilisation or embryo development
In Vitro Fertilisation
IVF is frequently regarded as the primary option for individuals seeking fertility treatment. While it is an effective and popular choice, IVF is more invasive, carries greater risks, and is costlier than alternatives such as Ovulation Induction and Intra-Uterine Insemination (OI/IUI). At Coastal IVF, we prioritise our patients’ needs and believe that IVF should be reserved for those who truly require it.
Coastal IVF boasts high success rates, and we are confident in our approach. That’s why we offer a second cycle guarantee, meaning minimal out-of-pocket costs for a subsequent cycle if needed!
IVF – The Process
- +/- Down Regulation
Various medications may be used to ‘quiet’ your ovaries and halt the normal cyclical recruitment of follicles. This crucial step ensures that we can stimulate as many follicles as possible at similar sizes. - Ovarian Stimulation
Injections of follicle-stimulating hormone (FSH) promote the growth of ovarian follicles, with the goal of developing ~10-20 dominant follicles by the time of egg retrieval. A second medication is often used to suppress premature ovulation. - Oocyte Retrieval (Egg Pickup)
Under anaesthesia, a long fine needle is used to carefully retrieve eggs from each follicle. - In Vitro Fertilisation and Embryo Culture
The retrieved oocytes are fertilised with sperm in the lab (via IVF or ICSI) and monitored for growth until approximately day 5, at which point they develop into ‘blastocysts.’ - Embryo Transfer
Usually 3-5 days after egg retrieval, embryos are transferred into the woman’s uterus, with the hope of successful implantation. - Luteal Support and Pregnancy Monitoring
Medications may be prescribed to support early pregnancy, and a blood test (b-hCG) is performed approximately 10 days after transfer to check for pregnancy.
Key requirements, pros and cons of IVF
-
- More demanding than OI/IUI
- Suitable for nearly all forms of infertility
- Higher success rates per cycle compared to OI/IUI
- Provides more diagnostic information than OI/IUI
- May require Intracytoplasmic Sperm Injection (ICSI) to assist fertilisation
Did you know? The landscape of reproductive techniques changed forever with the birth of Louise Brown in 1978, the world’s first IVF baby. Louise was born to a mother without fallopian tubes, highlighting the routine viability of IVF for patients with ineffective or failed tubal surgery.
Intracytoplasmic Sperm Injection
Intracytoplasmic Sperm Injection (ICSI) is a specialised fertility treatment in which a single sperm is directly injected into an egg to facilitate fertilisation. This technique is particularly beneficial for couples facing male factor infertility, such as low sperm count or poor motility.
Pros:
- Increases the chances of fertilisation when conventional methods are ineffective.
- Can lead to successful pregnancy rates comparable to those using normal sperm parameters.
- Eligible for Medicare rebates, making it more accessible.
Cons:
- ICSI is associated with a slightly higher risk of birth defects and there is a possibility of injuring the eggs during the injection process. However, when performed by experienced embryologists, the procedure is generally safe, and the overall risk remains relatively low in relation to its potential benefits.
- ICSI shares risks associated with assisted reproductive technologies, such as ovarian hyperstimulation syndrome (OHSS).
Consult your healthcare provider to discuss whether ICSI is the right choice for your fertility journey.

Testicular Sperm Aspiration
Testicular Sperm Aspiration (TESA) is a procedure designed for men with azoospermia, a condition where no sperm is present in the ejaculate. Performed under local anaesthetic, this technique involves extracting sperm directly from the testicle using a fine needle biopsy.
TESA offers couples who might otherwise require donor sperm the opportunity to achieve pregnancy using their own genetic material. This approach is particularly beneficial for men who have had a vasectomy or have conditions affecting sperm production (spermatogenesis). Before proceeding, the male partner must undergo initial investigations, which include a physical examination and blood tests.
TESA is the preferred biopsy technique for men with obstructive azoospermia, as it is less invasive than traditional open biopsy methods. It boasts a very low complication rate and allows for a quick recovery.
Frozen Embryo Transfer (FET) Cycle
Following a stimulated IVF cycle, couples often have surplus embryos that can be cryopreserved for future use. Frozen Embryo Transfer (FET) cycles provide an opportunity to utilise these stored embryos in a separate cycle.
The FET process begins with the preparation of the uterine lining (endometrium) to create an optimal environment for implantation. This preparation can be achieved through various methods, such as following a natural menstrual cycle, using ovulation induction techniques, or administering hormonal replacement therapy (HRT) to mimic the natural hormonal environment.
Once the endometrium is appropriately prepared, the frozen embryos are carefully thawed and assessed for viability before being transferred into the uterus. The goal of this procedure is to facilitate successful implantation, leading to pregnancy.
Recent advancements in freezing and thawing technologies, including techniques like vitrification, have significantly improved the outcomes of FET cycles. As a result, success rates for FET are now comparable to those of fresh embryo transfers, offering couples promising opportunities to achieve their dream of parenthood.
Pre-implantation Genetic Testing
Preimplantation Genetic Testing (PGT) is a cutting-edge procedure performed alongside In Vitro Fertilisation (IVF) to assess embryos for specific genetic abnormalities before they are transferred to the uterus. PGT-A (Preimplantation Genetic Testing for Aneuploidy) focuses on identifying chromosomal abnormalities, helping to select the healthiest embryos for implantation. PGT-M (for Monogenic disorders) is used in patients known to be at risk for a specific single-gene disorder such as Cystic Fibrosis or Spinal Muscular Atrophy.
Pros of PGT:
- Higher Success Rates: By selecting chromosomally normal embryos, PGT can increase the likelihood of achieving a successful pregnancy (per transfer) and reducing the risk of miscarriage.
- Reduced Risk of Genetic Disorders: PGT may help identify embryos that carry a genetic conditions, allowing couples to make informed choices about their embryos.
Cons of PGT:
- Increased Costs: The process of PGT incurs additional costs associated with genetic testing and laboratory procedures.
- Potential for Embryo Loss: The biopsy process, while generally safe, can result in the loss of some embryos, which is a consideration for couples with a limited number of viable embryos.
- Emotional Impact: The testing process can be stressful and emotionally taxing, as couples navigate the complexities of genetic information and its implications for their family planning.
Overall, PGT is a valuable tool for couples seeking to enhance their chances of a healthy pregnancy. It is important to discuss the benefits and potential challenges associated with PGT with your healthcare provider to determine if it is the right option for your fertility journey.
Make An Appointment
Please note that you require a referral from your GP to one of our doctors in order to access Medicare rebates.